How U.S. COVID Testing Strategy Will Extend Pandemic Nightmare
President Biden’s massive increase in home-based rapid antigen tests will lead to a tsunami of false-positive results, which will indefinitely extend the current “casedemic.”
The idea is to allow people to test themselves before attending social events, school, going to work, etc., so they can know, almost in real time, whether they may be infectious.
On its face, this seems like a reasonable approach. Why wouldn’t having more information about possible infections be a good thing?
Here’s why that’s actually a really bad idea. Mass testing of people who are overwhelmingly asymptomatic (showing no symptoms) will in fact inevitably extend this pandemic nightmare for additional months — maybe even years — as “cases” continue to mount from false positives (a test result that incorrectly identifies infection when none exists).
To be clear: Biden’s mass testing approach is exactly the opposite of what is needed right now. We should not be testing asymptomatic people.
The reason for this becomes clear only by looking beyond the headlines that claim skyrocketing cases and deaths from the infection.
The accuracy of the case, hospitalization and death numbers are a function of the accuracy of the screening tests we are implementing. Inaccurate tests will naturally lead to inaccurate data.
However, the distortion of these numbers is more than just a matter of the accuracy of our screening tests as will be explained below.
Though the public generally understands every test will have some amount of inherent error, we are told that the widely used COVID-19 tests are very accurate and thus we can trust the reports of “NEW CASES” shouted daily from most mainstream media platforms.
The reality is that even when a reasonably accurate test is used on a population that has a low background prevalence of active disease, the majority of positive test results will, in fact, be false.
Why is this the case? We must first examine what is meant by a test’s accuracy.
Sensitivity versus specificity — what’s the difference?
A test’s accuracy is defined by two things: its ability to diagnose a condition when it exists and its ability to rule out a condition when it doesn’t.
A given diagnostic test does not necessarily have an equal ability to rule in and rule out the condition it is designed to identify. For this reason, the accuracy of a test is defined by its sensitivity and specificity.
Sensitivity and specificity have precise definitions. A test’s sensitivity is the proportion of people who have a disease that the test will correctly identify with a positive result. In other words, if a test has a 90% sensitivity it will return a positive result nine times out of 10 when testing people with the disease.
Specificity is the proportion of people who do not have the disease that the test will correctly identify with a negative result. A test with 90% specificity will return a negative result nine times out of 10 when testing people who don’t have the disease.
Let’s demonstrate this further using an extreme example. Let’s say our test for diagnosing COVID-19 doesn’t involve PCR or antibody titers or antigen testing.
Instead, the test simply involves confirming that a person is alive.
If a person is alive, then in this hypothetical test, they must have COVID-19. If they are dead, they do not have COVID-19. Our hypothetical test’s sensitivity would be 100% because every person who has COVID-19 will test positive; no COVID-19 case will escape detection.
Obviously, this hypothetical test does not offer any meaningful information because every living person tested will test positive for the disease. Assuming we would test only living people, our test will never return a negative result.
In other words, this test will not identify anyone who doesn’t have the disease.
Another way of stating this is by saying that the specificity of our test is 0% because none of those who do not have COVID-19 will ever be identified.
The metric we really need to look at: positive predictive value (PPV)
The sensitivity and specificity of a given test do not change with the prevalence of the disease in the population being tested.
However, the proportion of false positives (people who do not have the disease but test positive) rises as the prevalence of the disease falls.
Though it may seem initially mystifying, this is an inescapable reality with any diagnostic test that is not 100% accurate. This is demonstrated below.
The ratio of the number of people who truly have the disease (true positives) compared to the number of people who test positive is defined as the positive predictive value (PPV) of the test.
Hence, the PPV of a test varies with the true incidence of the disease in the population being tested.
It is the PPV of a test that indicates the probability that a person who tests positive for a disease actually has the disease.
When one asks, “I tested positive for COVID. What are the chances I actually have the disease?” The PPV of the test is the answer they are looking for.
What happens when a reasonably accurate test is deployed upon a population that has a low incidence of disease?
The U.S. Food and Drug Administration describes it here. Using a test that has an impressive 98% specificity on a population where 1 in 100 actually have the disease (a disease prevalence of 1%) will result in a PPV of 30%.
In other words, 70% of those who test positive will not have the disease. Seven out of 10 will be false positives.
Now let us examine what will predictably happen when we deploy 500 million rapid tests on a population of people who are asymptomatic (which will be the case in the vast majority of circumstances in schools, social events, universities, workplaces, when traveling, etc.).
We must first estimate what the true prevalence of active COVID-19 is in the population. There are several ways to do this.
In their vaccine trial study published in the New England Journal of Medicine, Johnson & Johnson investigators found that of 43,783 participants, 238 tested positive by RT-PCR for SARS-CoV-2 infection (Supplemental Index, table S3) upon screening.
This constitutes a background active infection prevalence of 0.5%.
The authors cite the “… extraordinarily high incidence of SARS-CoV-2 infection” at the time of the trial as one of its strengths.
The trial was conducted during the spring and summer months of 2020. A higher prevalence of background active infections occurred in subsequent months.
Although the sample population is small compared to the population of the U.S. as a whole, national data support this number as well.
At the height of the pandemic, the Centers for Disease Control and Prevention (CDC) reported the seven-day rolling average of daily new COVID-19 cases was 250,440.
If we approximate the average bout of active COVID-19 is 10 days (the original recommended length of quarantine following a positive test), there were approximately 2.5 million active COVID-19 cases per 330 million people in the population on Jan. 11, 2021.
The peak active disease prevalence was therefore 0.75%. Throughout most of the pandemic the prevalence of the disease was considerably lower.
A Cochrane review of the rapid antigen tests promoted by the Biden administration states the tests’ sensitivity ranges from 58% to 78% in asymptomatic and symptomatic people respectively. The specificity also differs between the asymptomatic and symptomatic (98.9% and 99.5%).
However, these calculations are based on PCR tests as the reference. PCR tests are not 100% accurate either. Notably, unreasonably high cycle thresholds (Ct) were used throughout the pandemic which unavoidably led to more false positives and a lower specificity.
If we estimate these screening tests have an average sensitivity of 67% and a specificity of 98%, what will happen when these tests are administered on a population where the prevalence of the disease is not 0.5% or 0.75% but a very generous 1%? (It’s been far lower than this during most of the pandemic in the U.S., as explained above and discussed in this essay.)
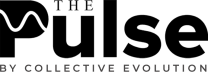
The chart below is from the BMJ online rapid antigen test (what the British call “lateral flow tests”) calculator. It shows 1,980 false positives for every 670 true positives, or a 75% false-positive rate.
This is the very definition of a “casedemic,” which is what happens when most cases are false positives or involve only mild symptoms.
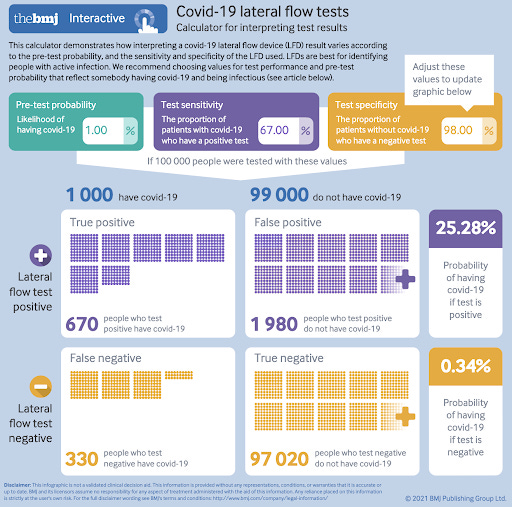
If we use more realistic assumptions of 0.5% disease prevalence and 90% antigen test specificity (due to user error and other frequent problems), we get a catastrophic 97% false-positive rate, with 9,950 false positives for every 335 true positives (see below figure).
This short essay in The BMJ, which appears as a “rapid response” to The BMJ online calculator, explains the scholarship demonstrating why testing asymptomatic people leads to massive numbers of false positives.
Sensible policy prescriptions to end the pandemic are presented in this essay, which discusses the need to change the COVID-19 “case definition,” to eliminate testing of asymptomatics and to lower the cycle threshold for PCR tests.
The remainder of this article will focus on why Biden’s approach to further increasing mass testing is the wrong way to go.
What is a case?
It is quite unusual (almost unique) that the CDC defines a “case” as a positive test result only. In the U.S., the vast majority of cases are identified and tallied based only on a PCR or a rapid antigen test result without any consideration of symptoms.
This approach can lead to very large numbers of false positives being misidentified as “cases.” This has been described as the “false-positive paradox” or the “false-positive catastrophe.”
When this trend goes too far we find ourselves in a “casedemic” rather than a pandemic.
To get out of a never-ending casedemic scenario, which is where we’re clearly headed, we need to be careful with our definitions, our testing procedures and our data tracking.
Singapore tracks symptoms and severity of all COVID-19 cases. As of data available through the end of December 2021, fully 99% of all Singapore “cases” were asymptomatic or mild.
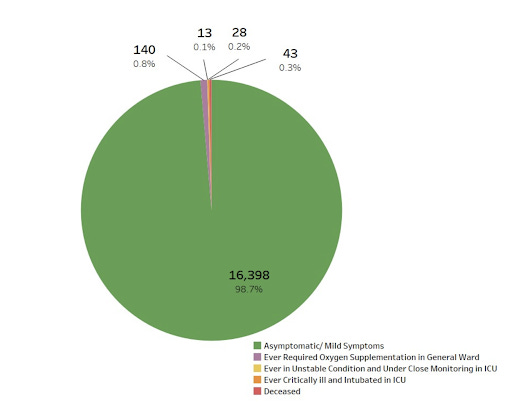
As a result of this overwhelming number of asymptomatic and mild cases, Singapore now focuses on hospitalization rates for tracking the severity of the pandemic, and in making pandemic policy choices.
Unfortunately, we don’t track asymptomatic/symptomatic distinctions in our public data here in the US. We’re still very much focused on “cases” of any sort, no matter how mild or asymptomatic.
Dr. Monica Gandhi at UCSF Medical School warned about this trend and urged the U.S. to adopt the Singapore approach by focusing on hospitalization figures rather than “cases.”
Gandhi said:
“Learning to live with the virus in the long term will require changes in both mindset and policy. Relying on COVID-19 hospitalizations as the most important metric to track closely will provide the most reliable picture of how an area is faring with the virus. And by focusing attention on the number of hospitalizations, health professionals can better focus on reducing them. This becomes especially important as case counts become more complicated.”
Given our focus on “cases,” we have in recent days reached even higher heights of Orwellian absurdity with respect to tracking and responding to the virus.
A recent Yahoo News article had the rather startling title: “What’s the difference between Omicron symptoms and cold symptoms? We asked an expert.”
The answer from the expert? Only a test can tell the difference.
To be entirely clear, if only a test can tell a cold and Omicron apart, then Omicron is just a cold.
The United Kingdom, with its record number of “cases” — most of which are surely false positives or extremely mild symptoms — promises to be a rehearsal for the U.S.
So get ready for an Omicron “casedemic” here in the U.S. — just like it’s unfolding now in the UK.
A recent CNBC story discussed UK data about Omicron symptoms, collected from a phone app over a wide number of “cases,” showing that Omicron symptoms are overwhelmingly mild and indistinguishable from the common cold.
And then … the article warned the reader not to underestimate Omicron or to mistake it for a cold.
There is now a good amount of data about Omicron and its symptoms and hospitalization rates. UK and South Africa data show it is extremely mild — basically a cold, and not even akin to a flu in terms of severity.
A number of other studies, as of late December 2021, support extremely mild symptoms and low hospitalization rates for Omicron cases, as reported by the New York Times.
Tim Spector, the UK scientist who developed the symptom-tracking phone app used in the UK, told the press:
“Broadly what we’re seeing now is the majority of people testing PCR positive actually have cold-like symptoms and they do not have the classical triad of ill COVID symptoms of fever, loss of smell and taste and persistent cough. So it’s slowly emerged into a more symptomatic milder condition that looks just like a severe cold to many people.”
It’s not just cases that are mild, it’s also fairly clear at this point the large majority of hospitalizations allegedly because of COVID-19 are in fact not related or are only minimally related to COVID.
Omicron hospitalizations in South Africa have been overwhelmingly a product of testing for COVID-19 upon entry into the hospital for any reason (i.e. no COVID-19 symptoms were showing), as a report from the South African Medical Research Council’s Dr. Abudullah stated:
“In summary, the first impression on examination of the 166 patients admitted since the Omicron variant made an appearance, together with the snapshot of the clinical profile of 42 patients currently in the COVID wards at the SBAH/TDH complex, is that the majority of hospital admissions are for diagnoses unrelated to COVID-19. The SARS-CoV-2 positivity is an incidental finding in these patients and is largely driven by hospital policy requiring testing of all patients requiring admission to the hospital.”
Yet despite all of the data overwhelmingly pointing toward Omicron being extremely mild and generally indistinguishable from a common cold, the linked CNBC article ended with this:
“We’re concerned that people are dismissing Omicron as mild. Even if Omicron does cause less severe disease the sheer number of cases will once again overwhelm health systems.”
Are we already in a ‘casedemic’?
“Overwhelming” health systems with COVID-19 cases, which are in the vast majority of instances false positives or mild symptoms, is the very definition of a “casedemic.”
The “cases” we were warned about in the CNBC article are, based on the UK data cited, overwhelmingly asymptomatic or very mild cold-like symptoms. And it is these kinds of “cases” that threaten to overwhelm the system with unwarranted “cases” and “hospitalizations” and the consequent panic that our irresponsible media and political leaders are sowing through their ongoing mismanagement of pandemic responses.
It is quite obvious that what is happening in the UK until recently was a massive increase in testing due to panic about Omicron, and a massive increase in false positives, which is inevitable when you ramp up asymptomatic testing with even accurate tests, let alone inherently flawed tests — which is what we have (PCR and antigen tests are both highly problematic for different reasons).
Harvard Medical School professor Westyn Branch-Elliman described in a US News & World Report essay how asymptomatic testing in school kids could lead to literally 71 out of 72 positive COVID-19 test results being false positives.
The same logic applies equally to all testing of asymptomatic people. With testing of asymptomatic people becoming extremely widespread in the U.S. and other countries, we are indeed seeing a tsunami of false positives.
Now with seasonal cold and flu making a comeback, many people are testing after showing cold or flu symptoms. When the large numbers of COVID-19 false positives inevitably occur, these people are tallied as confirmed “cases” for COVID-19, instead of the common cold or flu they actually are.
If we don’t get smart about these dynamics we will be stuck in an endless cycle of panic, increased testing, increased false positives, more panic, etc.
So what is the real impact of the pandemic?
Today’s narrative around Omicron continues the pattern of extreme exaggeration of all public COVID-19 stats, followed by the inevitable over-reaction from policymakers, politicians and the public.
Two years into this global nightmare it is becoming clear that the pandemic is overwhelmingly a man-made and policy-made event, where it is the policy choices themselves that are causing the vast majority of harm, not the virus.
As previously explained in detail, using reasonable estimates of PCR accuracy and a low prevalence of disease in the population being tested, it is a mathematical certainty that case counts will be highly exaggerated.
Combine this with testing that is routinely done on all patients upon admission, we arrive at the unavoidable conclusion that we have overestimated hospitalizations and deaths attributable to COVID-19 as well.
‘COVID-19 Deaths’ = Deaths WITH COVID-19, not FROM COVID-19
The reality is that it is very difficult, if not impossible, to arrive at a universally accepted and accurate method to differentiate a death “from” COVID-19 from a death “with” COVID-19.
For example, take a hypothetical patient with heart disease who contracts moderately severe COVID-19, gets admitted to a tertiary care center with COVID-19 symptoms and dies of a heart attack several days later.
Did that person die from COVID-19 or with COVID-19?
Clearly, the patient’s admission to the hospital was due to a SARS-COV2 infection. Would that person have died at that time if he did not contract COVID-19? Probably not.
On the other hand, would the individual have died if he did not have heart disease? Probably not. After all, the CDC reports that 95% of those who die from COVID-19 have one or more comorbidities.
It is reasonable to attribute the death, in this example, to COVID-19 and have it recorded as such. It is not reasonable to expect that our health authorities would be able to investigate every death during a pandemic and sort out which deaths are “more likely” the result of a SARS-COV2 infection and which are “more likely” due to underlying disease states.
In order to not underestimate the potential lethality of a SARS-COV2 infection early on, we may excuse the use of a broader definition of what constitutes a COVID-19 death.
However this approach inevitably resulted in nonsensical attribution of deaths to COVID-19. But how often?
State departments of health explicitly acknowledged this source of error early in the pandemic at a time when they were far more candid than they are today.
Illinois’s director of public health, Dr. Ngozi Ezeke, explained to reporters in April 2020, early in the pandemic:
“If you died of a clear, alternate cause but you had Covid at the same time, it’s still listed as a COVID death. Everyone who is listed as a COVID death, doesn’t mean that was the cause of the death, but they had Covid at the time of death.”
In order to put all questions to rest, Ezeke expanded on these definitions as follows:
“I just want to be clear in terms of the definition of ‘people dying of COVID.’ The case definition is very simplistic. It means, at the time of death, it was a COVID-positive diagnosis. That means, that if you were in hospice and had already been given a few weeks to live, and then you also were found to have COVID, that would be counted as a COVID death.”
https://www.facebook.com/watch/?v=611736272757614
There is no reason to believe that our health authorities have changed their approach in classifying COVID-19 deaths or hospitalizations. In fact, as explained above, it would not just be impractical, it would be impossible to do so.
So where are we now?
No, the U.S. didn’t recently pass 800,000 deaths “from” COVID-19, as is widely reported.
That figure is not remotely accurate because it includes all “deaths involving COVID-19,” as the CDC describes clearly in its data, and this definition includes all people where COVID-19 is implicated in any way or is merely suspected of “contributing to,” as opposed to causing, the death.
We must substantially downgrade this figure, not only because state health departments do not differentiate between “from” and “with” deaths, but also because published analyses support the hypothesis that hospitalizations and deaths are over-attributed to COVID-19.
In this peer-reviewed study from the American Academy of Pediatrics, 40% of hospital admissions had infections diagnosed incidentally and another 47% had only “potentially” symptomatic infections. A whopping 87% of COVID-19 hospital admissions were not due to COVID-19 in this survey.
In this large preprint study examining U.S. Department of Veterans Affairs hospital admissions, 36% to 48% had only mild COVID-19 symptoms. We can thus infer that these hospitalizations, in an adult population, were also not due to COVID-19 but to other underlying causes.
The same logic applies to “COVID-19 deaths,” suggesting strongly that “COVID-19 deaths” are equally exaggerated, just as Ezeke implied nearly two years ago.
The impacts from lockdowns, pseudo-lockdowns and related policies have indeed been massive and will continue to be destructive, especially for children, until we demand our authorities acknowledge the exaggeration inherent to widespread testing and the substantial proportion of hospitalizations and deaths attributed to COVID-19 that are clinically unrelated to infection.
Has Britain come to its senses?
Recently British PM Boris Johnson announced mask mandates will no longer be enforced in the commonwealth. The BBC reported COVID passes (proof of full vaccination or recent negative test) will no longer be required for entry into large venues.
At a recent Downing Street press conference, Britain’s Health Secretary Sajid Javid said, “This is a moment we can all be proud of. It’s a reminder of what this country can accomplish when we all work together.”
Is it really a moment to be proud, sir? Or are you finally admitting defeat?
Javid’s statement comes at a time when England’s new daily confirmed COVID-19 cases are 50% higher than the previous peak one year ago and daily COVID-19 hospitalizations remain higher than in the last 11 months.
With cases and hospitalizations at near all-time highs, what was accomplished? What exactly are the standards for success?
If anything, Javid is publicly acknowledging, through self-congratulatory remarks, that his administration’s approach has predictably and monumentally failed. Our friends across the pond have always had a knack for irony.
Apparently British authorities have finally recognized that vaccine passports, travel restrictions, mandates and most importantly, indiscriminate testing, do nothing to end a casedemic.
When will the U.S. admit the same? Not anytime soon it seems. Despite basic epidemiological concepts and evidence that point to the contrary, our authorities are implementing policies that will unavoidably perpetuate the casedemic in this country.
This work is reproduced and distributed with the permission of Children’s Health Defense, Inc. Want to learn more from Children’s Health Defense? Sign up for free news and updates from Robert F. Kennedy, Jr. and the Children’s Health Defense. Your donation will help to support us in our efforts.
Sign up for free news and updates from Robert F. Kennedy, Jr. and the Children’s Health Defense. CHD is implementing many strategies, including legal, in an effort to defend the health of our children and obtain justice for those already injured. Your support is essential to CHD’s successful mission.